As attacks on health care workers become increasingly more common, workplace safety experts are calling on regulators and employers to better protect those caring for patients.
Incidents spiked during the COVID-19 pandemic amid understaffed medical facilities, increased substance abuse and an overall lack of mental health services, experts say. And although the issue is on the radar of federal and state lawmakers and regulators, some say change isn’t happening fast enough.
“There’s been a substantial rise over the past few years,” said Mustafa Mufti, chair of the department of psychiatry at ChristianaCare Health System in Wilmington, Delaware.
Dr. Mufti points to pandemic-induced patient frustration, hospital staffing shortages, and increasing substance abuse rates all contributing, as is the broadening of the definition of violence to include verbal threats and intimidation. Biological factors, psychological factors and social factors all play a role, he said.
Restricted access for family members at hospitals during the pandemic also contributed, Dr. Mufti added.
“It’s been a very high period of intense emotion,” he said.
Akin Demehin, senior director of quality and patient safety policy for the Washington-based American Hospital Association, said nurses are the workers most often affected by workplace violence.
“Just given the flow of the work that happens inside of health care organizations, it really is nurses that tend to be in that uniquely vulnerable position,” he said.
The U.S. Bureau of Labor Statistics reports that health care and social service workers experience the highest rates of injuries caused by workplace violence and are five times more likely to suffer a workplace violence injury than workers in all industries.
In the second quarter of 2022, there were 1,739 nurse assaults a month, according to South Bend, Indiana-based patient safety organization Press Ganey.
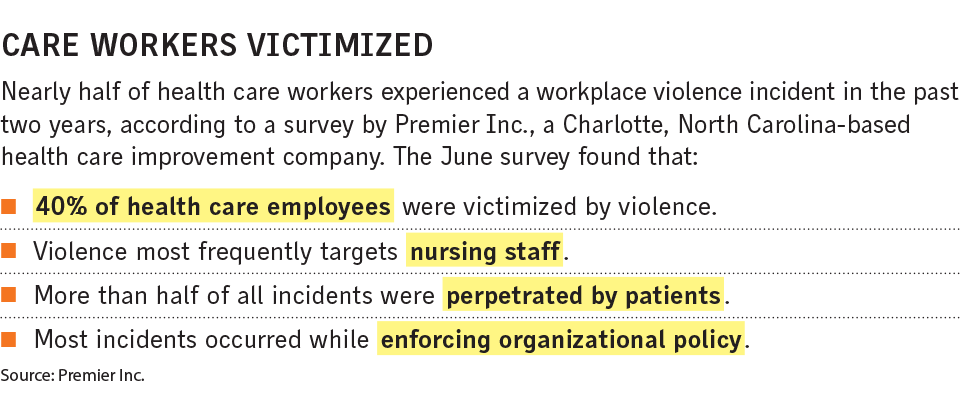
The assailants are often patients but also include family members, visitors and co-workers, according to Press Ganey.
An April 2022, National Nurses United survey showed 48% of hospital nurses reported increases in workplace violence, up from about 30% in September 2021.
The American Nurses Association reported that the most significant workplace risk for nurses this year has been stress and that as many as one in four nurses have been assaulted at work.
“Workplace violence in nursing is a longstanding issue that is unresolved,” Ruth Francis, ANA senior policy advisor for nursing practice and work environment, wrote in an email.
Ms. Francis said a lack of consistent and accurate data is a major barrier to implementing effective violence prevention programs, especially in states without workplace violence prevention laws. Many nurses assume patient abuse comes with the job, so they choose not to report incidents, she said.
Priscilla Ross, senior associate director of federal relations for the American Hospital Association, said facilities are trying to address the concerns.
“The vast majority of our hospitals have implemented programs and interventions to try to address workplace violence,” she said.
The Joint Commission, an Oakbrook Terrace, Illinois-based agency that sets standards for hospitals, implemented accreditation benchmarks for hospitals designed to address violence. They went into effect in January 2022 and apply to all Joint Commission-accredited health care facilities and critical access hospitals in the U.S.
The standards provide a framework for workplace violence prevention programs, including training and post-incident strategies.
The U.S. Occupational Safety and Health Administration has been trying to create a workplace violence in health care standard for years. An OSHA public comment period related to health care violence ended in July.
Attorney Wayne Pinkstone, with the Philadelphia office of Ogletree Deakins P.C., said the potential for an OSHA standard heightens the importance of the issue for employers and noted that some state laws already have compliance requirements regarding workplace violence (see related story below).
There are also administrative controls that can be implemented, such as increasing staffing numbers and requiring workers to promptly report workplace threats, experts say.
Federal lawmakers are also working to address the issue.
One bill, to establish the Safety From Violence for Healthcare Employees Act, sponsored by U.S. Rep. Madeleine Dean, D-Pa., would establish criminal penalties for knowingly assaulting or intimidating hospital personnel, similar to existing measures related to assaults on airline workers.
The bill also calls for $25 million in grants for education and training for health care facilities.
“We have to lift up the issue and do what we can to protect health care workers,” Rep. Dean said.
States pass laws aimed at strengthening protection for nurses
As workplace violence incidents against nurses rise nationwide, states are taking much of the lead on mitigation efforts.
Many states already require health care employers to conduct hazard assessments and implement security measures such as installing metal detectors, physical barriers and door locks to reduce exposures, said Wayne Pinkstone, an attorney with the Philadelphia office of Ogletree Deakins P.C.
Eleven states have laws requiring health care employers to establish workplace violence prevention plans, according to the U.S. Occupational Safety and Health Administration. They are California, Connecticut, Illinois, Louisiana, Maine, Maryland, Nevada, New Jersey, New York, Oregon and Washington.
The rising workplace violence against nurses spurred the passage of Washington state Senate Bill 5454, which makes post-traumatic stress disorder a compensable occupational injury for nurses. The law takes effect in 2024.
Katharine Weiss, director of government affairs for the Washington State Nurses Association, said advocates brought the issue to legislators’ attention last year after several members were diagnosed with work-related PTSD but were denied workers comp benefits.
“It just really put a microscope on those already pre-existing issues, like short staffing,” she said.
In 2020, Pennsylvania state Sen. Maria Collett, who is a nurse, cosponsored a bill that was signed into law that permits nurses to leave off their last names from work ID badges to prevent stalking.
In June of this year, Pennsylvania legislators filed H.B. 1088, which would require hospitals, long-term-care nursing facilities and home health care agencies to develop workplace violence prevention committees to better protect employees.
“Physical violence and verbal aggression in the workplace are never OK, but in a health care setting, this has the potential to compromise the quality of care and safe staffing levels,” said Pennsylvania state Rep. Ben Sanchez, a supporter of the bill.




More Stories
Ashwagandha’s Impact on Cortisol Levels in Stressed People
Health care cyberattack ‘likely one of the worst,’ expert says
Accessing Medicinal Cannabis in the UK: A Comprehensive Guide